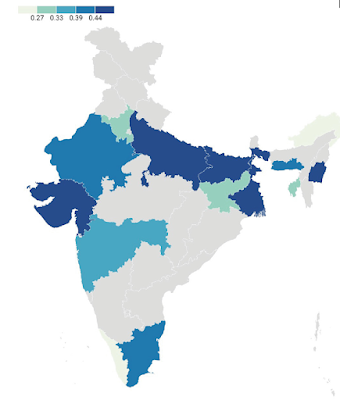
Geographic distribution of the G allele
(TIMPRSS2), which is associated with
a higher death rate from COVID-19. It’s most frequent on the Indo-Gangetic Plain,
which has the longest continuous history of urban settlement in South Asia. Did
that environment select for susceptibility to coronaviruses as a way to boost
resistance to deadlier respiratory viruses?
The
common cold is caused by over 200 strains of rhinoviruses, coronaviruses,
adenoviruses, and enteroviruses. Coronaviruses differ from other respiratory viruses
in one key respect: they can enter lung tissue via the ACE2 receptor. So if that receptor is altered to allow easier
entry, the host would become more susceptible to the common cold but not to
other respiratory diseases, including much deadlier ones that cause
tuberculosis, pneumonia, or pneumonic plague.
The
last point is important because there is evidence that a viral infection can
protect against subsequent infection by respiratory viruses. When mice are
infected with γherpesvirus 68, which is similar to Epstein-Barr virus, there is
production of large quantities of IFN-γ and activation of macrophages that
protect against Listeria monocytogenes
(which causes listeriosis), Mycobacterium
tuberculosis (which causes tuberculosis), and Yersinia pestis (which causes bubonic and pneumonic plague) (Barton
et al., 2007; Miller et al., 2019). A cytomegalovirus infection likewise
protects against Listeria monocytogenes
and Yersinia pestis (Barton et al.,
2007).
Coevolution
between coronaviruses and early urban settlement
Beginning
some 10,000 years ago, hunting and gathering gave way to farming, and nomadism
to sedentism. People began to live in progressively larger settlements along
the Nile in Egypt, the Tigris and the Euphrates in Mesopotamia, the Indus and
the Ganges in northern India, and the Yellow and the Yangtze in China. That is where
large numbers of humans first lived in close proximity to each other, and they
were particularly vulnerable to the spread of respiratory diseases from one
person to another. There may thus have been selection among them for increased
susceptibility to coronaviruses, which are normally mild in their effects, as a
means to increase resistance to deadlier respiratory viruses.
A
recent Indian study by Pandey et al. (2022) suggests that coronavirus
susceptibility may have coevolved with risk of infection by life-threatening
respiratory viruses like tuberculosis, pneumonia, and pneumonic plague, at
least in South Asia. People are more susceptible to infection by coronaviruses
if they have the G allele of the TMPRSS2
gene. The research team found that the G allele is significantly associated
with a higher fatality rate for COVID-19, apparently because it helps coronaviruses
enter lung tissue via the ACE2
receptor.
Pandey
et al. (2022) also charted the geographic distribution of the G allele in South
Asia. This allele is most frequent among inhabitants of the Indo-Gangetic Plain,
i.e., the fertile lowlands that border the Indus and Ganges rivers of northern
India and Pakistan. This is also where urbanization has existed for the longest
continuous time in South Asia, specifically since the early first millennium
BCE. The Indo-Gangetic Plain has had "an uninterrupted sequence of
economic development, state formation, and cultural expansion affecting the
entire subcontinent as well as Central, East and Southeast Asia" (Heitzman
2008, pp. 12-13).
These
findings are roughly consistent with an earlier finding by the same research
team. Srivastava et al. (2020) found that an ACE2 allele, at rs2258666, has a negative relationship with the
fatality rate for COVID-19. It is also most frequent in the northeast of India,
which until recent times was sparsely populated, and whose inhabitants lived in
dispersed rural settlements.
References
Barton,
E.S., D.W. White, J.S. Cathelyn, K.A. Brett-McClellan, M. Engle, et al. (2007).
Herpesvirus latency confers symbiotic protection from bacterial infection. Nature
447:
326-329.
https://doi.org/10.1038/nature05762
Frost,
P. (2020). Does a commensal relationship exist between coronaviruses and some
human populations? Journal of Molecular
Genetics 3(2): 1-2.
Heitzman,
J. (2008). The City in South Asia.
London: Routledge
Miller,
H.E., K.E. Johnson, V.L. Tarakanova, and R.T. Robinson. (2019). γ-herpesvirus
latency attenuates Mycobacterium tuberculosis infection in mice. Tuberculosis 116: 56-60.
https://doi.org/10.1016/j.tube.2019.04.022
Pandey,
R.K., A. Srivastava, P.P. Singh, and G. Chaubey. (2022). Genetic association of
TMPRSS2 rs2070788 polymorphism with COVID-19 case fatality rate among Indian
populations. Infection, Genetics and
Evolution 98 https://doi.org/10.1016/j.meegid.2022.105206
Shirato,
K., M. Kawase, and S. Matsuyama. (2018). Wild-type human coronaviruses prefer
cell-surface TMPRSS2 to endosomal cathepsins for cell entry. Virology 517: 9-15.
https://doi.org/10.1016/j.virol.2017.11.012
Srivastava,
A., A. Bandopadhyay, D. Das, R.K. Pandey, V. Singh, N. Khanam, N. Srivastava,
P.P. Singh, P.K. Dubey, A. Pathak, P. Gupta, N. Rai, G.N.N. Sultana, and G.
Chaubey. (2020). Genetic Association of ACE2 rs2285666 Polymorphism with
COVID-19 Spatial Distribution in India. Frontiers
in Genetics. September 25
https://doi.org/10.3389/fgene.2020.564741






5 comments:
Peter, now that COVID is ending (becoming endemic with Omicron), will the world go back to normal (i.e. the pre-2020 status quo), or has something changed? Was COVID a one-off event, or is it actually a sign of what could continue to cripple societies? Also, do you see any evidence that COVID could be "nature's response" to a world that's gotten too diverse and interconnected? While it existed, COVID gave the US the ability to reduce immigration, which would have otherwise been impossible in today's PC culture (deportations have become unacceptable). To the extent that it's ending, the future of America's "Title 42" allowing quick deportations of migrants at the border due to a health emergency could also be in question.
It's not a one-off event. There will be another global pandemic, and each successive pandemic is spreading more quickly and more globally than the previous one. The underlying problem is that (1) more people are travelling internationally and (2) border controls have become more relaxed. This increase in human mobility, together with the increasing size of the world's population, has created a tinderbox that pathogens will exploit within increasing ease.
Will the world react by closing up and separating? When Omicron escaped from South Africa, people bristled at the idea of restricting travel from there, even for a short period of time, which I found crazy. For some reason, the modern world is hysterically opposed to any kind of isolation or closed borders. They call it "insulting" or "unethical," and borders have become "racist." Will that attitude have to change?
Eventually, that attitude will have to change, but "eventually" might be a long time.
Few people change their minds overnight, especially if they have invested a lot of effort in promoting a particular mindset. There is one cause for hope: the elites have been disproportionately hurt by the pandemic because they tend to have a global, jet-setting lifestyle.
Very Insightful..Thank You for writing this wonderful blog on our research
Post a Comment